I’m probably most excited about being back up and running again on the interwebs because of this one post, right here: an interview with Susan E. Ingebretson, author of FibroWHYalgia: Why Rebuilding the Ten Root Causes of Chronic Illness Restores Chronic Wellness.
(Please note: All product links are affiliate links. That means you pay exactly the same amount, but I get a little bit for your purchase, which helps me keep this site going to bring you all more great stuff like this post!)
I’ll be reviewing the book in a subsequent post. Right now, grab a cup of coffee (or even better – green tea) and meet your newest fibro-friend and mine — Sue Ingebretson.
Sue, thanks so much for doing this. Tell us how you got “introduced” to chronic pain, personally.
I think I’ve had the “typical” fibro body since puberty. I didn’t know it then, but the difficult menstruation, digestive troubles (that’s a kind way to refer to the intestinal tornado), dark under-eye circles, etc. all reflect someone starved of nutrition. That, paired with my environmental exposures to toxins (farm chemicals) made for a likely path of pain. I don’t believe it’s coincidental that my first exposure to dental mercury and my first experience with IBS came at the same time. Stir in the mix of hormones, and there’s a recipe for pain and general poor health.
My first experience with chronic pain came at age 15 after a school bus accident. The bus went off a bridge (swung off with the front axle stuck on the guardrail and the rear of the bus stuck on the creek bank). I was lucky to have only suffered a concussion and a broken nose. However, relentless pain followed that event for several years. It just sort of faded away in my early 20’s as a new mom I became “too busy” to pay attention to it very much (of course that’s an over-simplification). I was aware of chronic low back pain, but just thought it would be with me for life.
It seemed to wax & wane depending on circumstances and other injuries. The IBS, however, never really went away.
Had you ever known anyone with chronic pain before your symptoms started?
During my school years my mom was always sick. Now we know she suffered (needlessly) with terrible food and environmental allergies. At the time, though, it was awful seeing her cough, sneeze and walk hunched over from pain. I’m sure that today, she would be diagnosed with fibromyalgia. At that time, the doctors were terrible to her. Small town doctors gave her very poor advice.
What prompted you to write this book?
I was active in my writer’s group working on various children’s projects. I’ve always loved writing for children and teens. As I succeeded in my personal journey to get healed, I found myself speaking on the subject as well as answering many desperate phone calls and emails. I told my writer’s group that various projects were on hold pending this or that speaking engagement. It finally became apparent that I needed to write down my experience, so I could give people a bigger picture of healing rather than a 30 minute phone call or back and forth emails. I intended to write a quick “health pamphlet” and be done with it. Instead, it took three years and ended up as a book.
In the book, you write (very humorously, I might add!) about your myriad experiences with the medical profession in seeking a diagnosis — what I call “the bad doctor stories.” Were you satisfied with your response to the “bad” doctors — the ones who dismissed you, the one who told you to be grateful you didn’t have heart disease — I especially liked the one who told you that you were afraid of getting older! Anything you wish you’d have said or done in retrospect? Or, alternatively, any advice for people currently seeking diagnosis who are dealing with their own “bad doctors”?
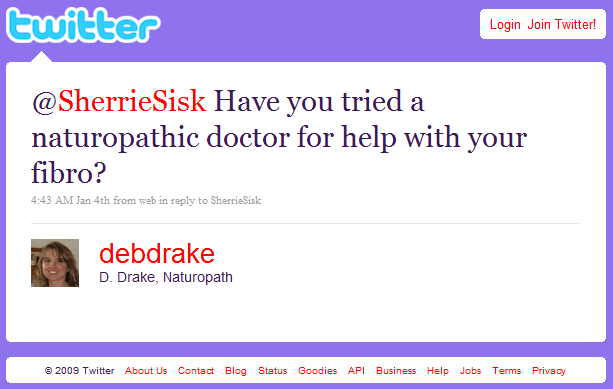
I have lots of things I’d like to say to my “bad” doctors, but I won’t. It makes me think of a friend who has a t-shirt that says, “I’m a writer. Be nice to me or you’ll end up in my next novel.” [NB from Sherrie: HA! I totally am stealing this.] There’s something to be said of writing down your injustices, however, I have no intention of giving them my book and saying, “So there.” I doubt it would make much difference. I just feel better myself for getting it out there. I’ve heard hundreds of stories from others who all have their share of similar (and/or much worse!) stories. The thing is, many doctors are simply working with the limited knowledge that they have. Very little is discussed in medical school about autoimmune conditions and about fibro. They’re tough to nail down (diagnostically) and tough to teach. It takes a dedicated doctor who is interested in and/or specializes in neurological and immune system conditions.
My advice for anyone dealing with doctors is to be as business-like and prepared as possible. When you give vague information, don’t be surprised at vague responses. Go with notes & questions. Ask for a specific action plan. If you feel your voice is not heard, move on! Find another doctor who will listen. They are out there.
We frequently hear “it’s all in your head” — which, as you point out, is somewhat accurate, since that’s where our brains are located, generally speaking (I wouldn’t presume to generalize, of course…). I have a theory that this phrase has become such a hot-button issue with the chronic pain/fibro community that we reject the very measures that could help us – meditation, cognitive behavioral therapy, even antidepressants — because we think we’re being told the pain has no biological cause, which of course isn’t true at all. In a manner of speaking, we’re at risk of cutting off the nose to spite the face. What do you think of my theory?
I agree with you, and here’s why. We all agree that stress is a HUGE factor in fibro, right? Where does stress originate? From thoughts, the brain. You don’t say, “my pinkie finger hurts, it must be stressed.” Stress is a mental/emotional component of illness that has VERY physical results. The thoughts/emotions are real, and so are the symptoms. The conflict comes from the (erroneous) perception that if it’s as simple as a thought, we could stop it or somehow have control over it. We can, in a way, but it’s not simple at all.
Stating that any condition is “all in your head” implies CHOICE. We choose to be sick. We choose to watch our bodies physically fall apart. That’s just silly. No one would choose that. The problem is that some of our actions are exacerbating our symptoms and it’s a learning process to find out what to do about it. Cognitive Behavior Therapy can be very impactful. I just took part in an 8 week CBT study that I found fascinating. Everyone in the group had positive results and I look forward to seeing the study published.
Again, the hot-button issue comes from the insinuation that we could do something about the condition if we only wanted to. There’s kernel truth to that, but not in the way that it’s meant. The comment is a hurtful, and non-productive jibe.
What’s funny is that I now feel so confident in my understanding of why I have fibromyalgia, that I don’t take comments like that personally at all. I’ve been in groups where others get fired up about the legitimacy of their condition. I don’t give a hoot. If someone wants to rant about fibro not being real, that’s their issue, not mine. I know exactly what I have and I take seriously my responsibility (to myself) to do something about it (self-care). I’m not personally offended at all by what I see as ignorance in others.
How can those of us who’ve been at this particular dance for awhile now best help those who are just getting here? What can we do better to advocate for and help the newly-diagnosed get the treatment they need? To put it a different way, how can we empower the newly-diagnosed fibromites?
I love this question! First thing is to blow away the mis-information found in media, doctors, articles, etc. that tell newbies of their dire future. That simply is NOT the case. I know many, many people leading full, busy, productive lives with fibro and other chronic conditions. The body is DESIGNED TO HEAL! YAY!
I had a friend once with a temperamental sports car. He knew it so intimately that he could tell by the sound of the engine what it needed. He lovingly cared for that vehicle and it served him well with nary a hiccup. Too many of us treat our bodies as vehicles that should always go when we step on the gas — never mind that there’s no fuel in the tank and there’s never been regular maintenance.
Another big misconception is that fibro is degenerative or progressive. It is NOT. The condition may progress or worsen IF the body is not cared for and allowed to deteriorate. That would happen to anyone. What if we took a completely healthy person, put her in bed most of the time, fed her foods with little to no nutritive value, and asked her to think constant negative thoughts. What would happen to her body? Would she deteriorate? The body needs oxygen, movement, nutrition, hope for a positive future.
Guess I got off on a tangent, but I am passionate about grabbing the newbie before he or she can be indoctrinated into the Eeyore thought process that nothing will change. A body in pain is an intelligent body. It’s telling you (OK, maybe screaming at you) that something is wrong. Something needs to be fixed. Only you can determine what that is and get to work.
On another note, I’ve personally experienced and seen that fibro in newbies has a better chance of diminishing or being next-to-non-existent once they figure out what to do to fix it. (I never say it permanently goes away). I’ve seen people who have not been ill that long, go on crusades to fix their bodies and do very, very well. That was the case for me and I was symptom-free for quite a while. Maybe a year or two? Then I slacked off on my health maintenance and took my wellness for granted. The fibro came back during a time of extreme stress. It’s never come back nearly as bad as it was before, but it’s still there — just a wee bit.
So — there again — I encourage newbies to take charge, take action, and figure out your own game plan!
In your book, you advocate a “cleaner” diet (more organic, lower on the food chain) and exercise as the starting point for a fibromyalgia treatment plan. How can those of us who are suffering economically and those of us particularly prone to post-exertional malaise begin to implement these lifestyle changes?
I can only speak for myself and from the experience of others I’ve seen, but repairing a body nutritionally has profound results. The same goes for fitness, but I’ll start with foods.
It’s been my experience that healthier foods can be much cheaper. Boxed, packaged, processed foods are pricey. You’re paying for the packaging and advertising, not the products. Processed foods are made of the cheapest ingredients on the planet. Water, HFCS, trans fats and artificial flavors and colors are the main four ingredients in almost all packaged foods. They’re cheap (for the manufacturer) and a source of empty, crappy calories.
I always say to buy the best quality foods and supplements that fit within your budget. Understandably, not everyone can buy always buy organics. But it’s a trade-off. Maybe you can choose the organic broccoli and pass up the toaster waffles? It’s all up to you. For me, it was a long process. I had to learn to value my body and decide that it was worth the “better” ingredients. Again, better does not always mean more expensive.
I go into detail in my book about soup. It’s about the cheapest thing you can make. Healthy, satisfying, nutritious. Beans are cheap, too. Produce can be. I can go to a local swap meet and come home with bags of produce for under $15. Maybe you can seek out local markets? Local growers? Better yet, make a small garden a family project this summer. You can’t get a cheaper food than buying it from seed. I’m no expert, but I’m told many veggies grow abundantly with very little care.
As far as fitness goes, my theory may be controversial. I believe that you have to keep moving. Yes, I know it hurts. I used to hurt (terribly), too. I believe that the more fit you are, the more oxygen you pump through your body (fibro people are shallow breathers), the healthier you will be. Start out slowly, but KEEP GOING. Don’t stop. Obviously, you don’t want to cause physical damage — especially if weight is a significant issue for you — but seek out fitness routines that are non-impact. Simply jiggling on a mini-trampoline is powerfully healing for both the body and the mind. Remember that the brain gets a big boost from exercise, too. Tai chi has been around for a bajillion years for good reason. It’s non-impact and provides a great body/mind benefit.
Try walking, Wii, ping pong with the kids, swimming, the gym, etc. Whatever you do, make it routine, meaning do it regularly. Vary your activities so you’re not doing the same thing each time and keep going. Grab a friend for accountability. Write down your goals (and sign it!). Chart your progress. Whatever you need to do to motivate yourself. It doesn’t take much exercise. Even 15 minutes a day 3 or 4 times a week is better than nothing. Exercise and eating right is your way of telling yourself that you are important enough to care for. YOU have value!
I love the whole book – and I’m totally not just ass-kissing here – but I think my favorite part is where you discuss the “perfect environment” for fibromyalgia to flourish. “Talk” a little more about that.
You’ll probably note that I really say the same thing in my book over and over in different ways. Different people need to hear messages differently. I wrote that part in sort of a knee-jerk reaction to several people I was “dealing” with at the time. As I mentioned, I’m often referred by others with fibro, so I used to get a lot of phone calls and emails (I now try to limit it to email). Anyway, that section is sort of an amalgam of a couple of people I was dealing with. They said they wanted health. They said they wanted to get better. But their actions did not reflect that. No one wants chronic illness, but many people are surprised to learn that what they’re doing is making what they already have much worse. I sort of hold a mirror up to that. They might not always see a reflection that they like (and they might not be happy with me), but it’s meant to encourage and educate. In all things, I try to affirm people. BTW, I see myself in that reflection, too.
You write about achieving balance in Chapter 4 and later in the book as well, but balance isn’t a static condition, of course – it’s a constant series of readjustments, and sometimes we need to play both sides of the extremes in life. Where do you stand on the question of “honoring your limits” or “pushing beyond those limits”?
Boy that’s a good question. I had to learn (the hard way) to set personal boundaries. I had to learn when to say no to others and when to say yes to myself. That’s a tough lesson for many moms, in particular. At the time when I discovered “balance,” that was quite the novel idea for me. I thought I was only worth what I could produce or do. I didn’t see any value beyond that. That’s where balance comes in. My view of balance 5 years ago looks nothing like balance for me today. Now, I am much more relaxed, calm, content. It’s a long twirly path.
It took quite some time to hear my inner voice tell me when I was honoring my abilities and when I was not. It’s a learned process. It’s not really one that’s easy to teach. It’s a self-guided journey.
I see your “pushing beyond those limits” comment in two ways: physically through exercise, and physically/emotionally through activities. I do believe in pushing yourself through fitness to places beyond your belief system. When I walked with a cane, I certainly did NOT believe I could become a gym rat and lift weights 6 days a week (I no longer do that, by the way, and need seriously to get back to it!).
The point is that my belief system told me that my body was broken and had limitations. Only by experimenting and challenging those perceptions did I learn that they were not accurate. No one could tell me that, no one could show me that in a book, or teach it in any way. I had to learn that for myself.
And, for physical/emotional activities, I make planned, pragmatic choices about the activities I participate in. This past weekend, I attended a 3 day expo about an hour away from home. The drive each day, the full schedule of workshops, and the stress it brought was absolutely exhausting. However, it was a health expo that I thoroughly enjoyed it and felt it was worth the battering my body took. I did push beyond my limitations because I deemed it important and valuable. It passed my personal benchmark for importance. Would I have done that for a Star Trek convention? Not on your life!
All I can say is that challenges are good. How can we know what we can do without challenging ourselves to do it? I have a friend who was significantly overweight for much of her life, and now runs marathons. She’s an amazing example of a person who has challenged her own self perceptions.
What do you think it is about fibromyalgia that makes one person’s treatment another person’s waste of energy and money? Why can’t one treatment rule them all?
We are all so very different. From a personality standpoint and physiologically speaking. We each react to foods differently. We react to experiences differently. There are more factors causing us to be unique than causing us to be the same. We’ve sort of taken on the erroneous idea that meds and treatments are a one-size-fits all solution. Go down a pain relieving aisle at the drug store and see how many different headache remedies there are. Some feel Exedrin is best, for others it Advil, or Tylenol. We each metabolize what we take internally in our own way. That’s why nutrigenomics is so exciting to me. It’s exciting to think of a field of medicine that is tailor-made for me, specifically. It’s a growing study.
The sad thing about fibromyalgia patients is that they’re often “sold” treatments as something that works for everyone. Then their pain is compounded by feelings of failure. As if they’ve personally done something wrong.
There is NO ONE treatment that works universally. There are many healing factors that work for most, if not all, like what I call the Restoration Trio (nutrition, fitness, stress-relief/emotional wellness). But even within those treatments there are a myriad of options available. That’s why it’s so important to figure out what works for you. The only way to do that is to create an action plan. Do something!
What’s the best advice you’d give to someone in the throes of a horrid flareup? Starting with the first moments, what two or three things will bring relief to most?
First of all, thanks for spelling “throes” correctly. That makes me smile. Can’t tell you how often I see “throws of a flair up.” For a writer, that’s enough to send me into a flare!
Back to the flareup — it’s important to immediately calm yourself with whatever methods work for you (non-food related, please). First and foremost, tell your mind “stop!” Stop the emotions or whatever it is that now surround the flare. Tell yourself that you are now going to reverse the momentum you have and go back toward better times (less pain). Take a walk, especially in nature. Play Clue or Boggle with your kids. Take a bath or read a favorite book. Take a swim. Nourish your body inside and out with healthy food and a healthy environment cleared of clutter, etc.
When you feel your heart rate begin to settle down, tell yourself that the moment of “panic/worry/stress/anxiety” is over. It’s now time for recovery. Breathe deeply. No self-recriminations. No mental should’s or shouldn’ts. Remind yourself that this period of recovery is necessary to heal. Even if it’s just 15 minutes, your body is telling you that it needs to come first.
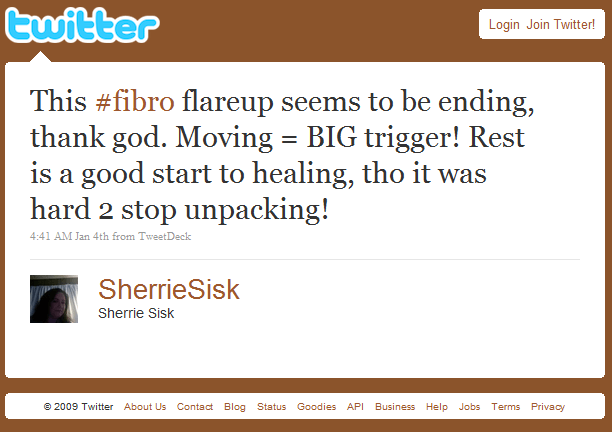
Later on, it’s very important to analyze what caused the flare. Most often, it’s obvious, but others not-so. If it’s an obvious thing, make an action plan for how you will avoid that in the future. If your flareup was caused by other people, you can’t always avoid them, but you can avoid how they affect you. That’s within your jurisdiction.
If it’s not so obvious, do some detective work. Consider your foods or environment. Look back at what you ate and where you were. I’ve had flareups and then realized that a gardener had fertilized the grass. Or that I’ve eaten a salad in the restaurant, and suspect toxic ingredients in the dressing.
Learning how to avoid flareups is the best solution of all. I know that’s a “Duh Barbie” statement, but it’s true.
What’s next for Sue? Will you write another book? Will you keep blogging at Rebuilding Wellness?
Yes, I plan to keep blogging — in fact that’s what I should be doing now! [NB from Sherrie: You can also catch more of Sue’s more frequent writings at the FibroWHYalgia Facebook page.]
I have many other projects planned and speak locally and do workshops. I have three workshops set up for April and May as well as some blogtalk interviews.
I’m very fortunate to have a wonderful connection and relationship with Cal State Fullerton. I’ll be developing workshops for them which will result in a workbook to go along with FibroWHYalgia. I’d love feedback on what others would like to see in such a workbook. I’m also working on a book of encouragement for those with chronic illness. It’s a short book with affirmations, Bible verses, etc. written to encourage and support people who wish to make positive change in their lives.
You’re totally doing God’s work, you know that, right?
I do remind myself of that daily. It’s not my message, it’s all His. In fact, at my book launch, I had my pastor pray over the book that it will touch softened hearts that are ready to heal. I wanted my book prayed over before it went anywhere! This message is not about me. God is using my experience to help me help others (gee, that sounds Jerry Maguire-ish. Help ME, help YOU!). You know what I mean!
Indeed I do.
* is a must-have addition for any fibromite’s library. Ingebretson’s personal history with the illness illuminates with good humor and compassion a difficult topic for all chronically ill people: the role of personal choices in the recovery process. Packed with solid scientifically-supported advice wrapped in a common-sense approach, FibroWHYalgia will help any fibromite thrive.